Our 2024-2025 Year in Review showcases key achievements over the past year as we work to deliver better health, together.

Message from our Board Chair Dr Richard Choong and CEO Bernie Kenny
We are pleased to share the progress WA Primary Health Alliance (WAPHA) has made in 2024-2025 towards advancing our vision of better health, together. This year was defined by strategic alignment, collaborative partnerships, and a focus on inclusion and data-driven decision-making in the context of the ambitious Australian Government primary health care reform priorities.
Our region – Western Australia
![]()

Australia’s primary health care commissioning landscape continues to evolve in response to national reform priorities, local needs and system-wide challenges.
As one of WAPHA’s core functions, we are responsible for planning, guiding and directing investment towards important primary health care services on behalf of the Australian Government. We work at a regional level to commission services which meet the unique and specific needs of our local communities and focus our efforts on areas where our work can most improve people’s health outcomes.

More than $233 million
invested and 290 services funded to improve the health and wellbeing of Western Australians.

27,655
clients received mental health support from commissioned services through 199,880 occasions of service*.

3,399
clients received support from commissioned alcohol and other drugs services through 21,375 occasions of service.
1.3 million
views of our black puppy depression campaign.

118,534
presentations across WA’s eight Medicare Urgent Care Clinics.

2,326
Aboriginal clients received support from commissioned mental health services through 19,500 occasions of service.
Note: *An occasion of service (service contact) is defined as the provision of a service by a PHN commissioned service provider for a client where the nature of the service would normally warrant a dated entry in the clinical record of the client.
Directing investment through need, capacity and supply
WAPHA’s investment decisions are guided by a structured commissioning model that integrates population health needs, identified through out comprehensive needs assessments, workforce capacity, and service supply.
During compilation of needs assessments, detailed analysis is undertaken for each of the PHN pillars, considering a wide range of information related to community need, local health care supply and workforce across WA. This is then triangulated to identify areas of high community need but lower levels of supply/workforce, enabling targeted investment in regions and populations most at risk of poor health outcomes and where we can have the most impact.
In addition to needs assessments, WAPHA undertakes population health planning activities throughout the year, including monitoring of local health needs, identifying populations and locations with unmet need, and conducting standalone needs assessments for topics as required.
This year, we published our Needs Assessments for the multicultural access, homelessness support and after-hours programs. The needs assessments included consultation with more than 110 stakeholders, including peak bodies, consumers and specialist support services, along with detailed data analysis to understand the after-hours, multicultural access and homelessness primary health care needs across WA, and provide recommendations to support potential service commissioning.
More than simply procurement of services
Commissioning is a continuous cycle that involves planning, designing or procuring, monitoring and evaluating health services to make sure they are performing well and improving the health outcomes of our communities.
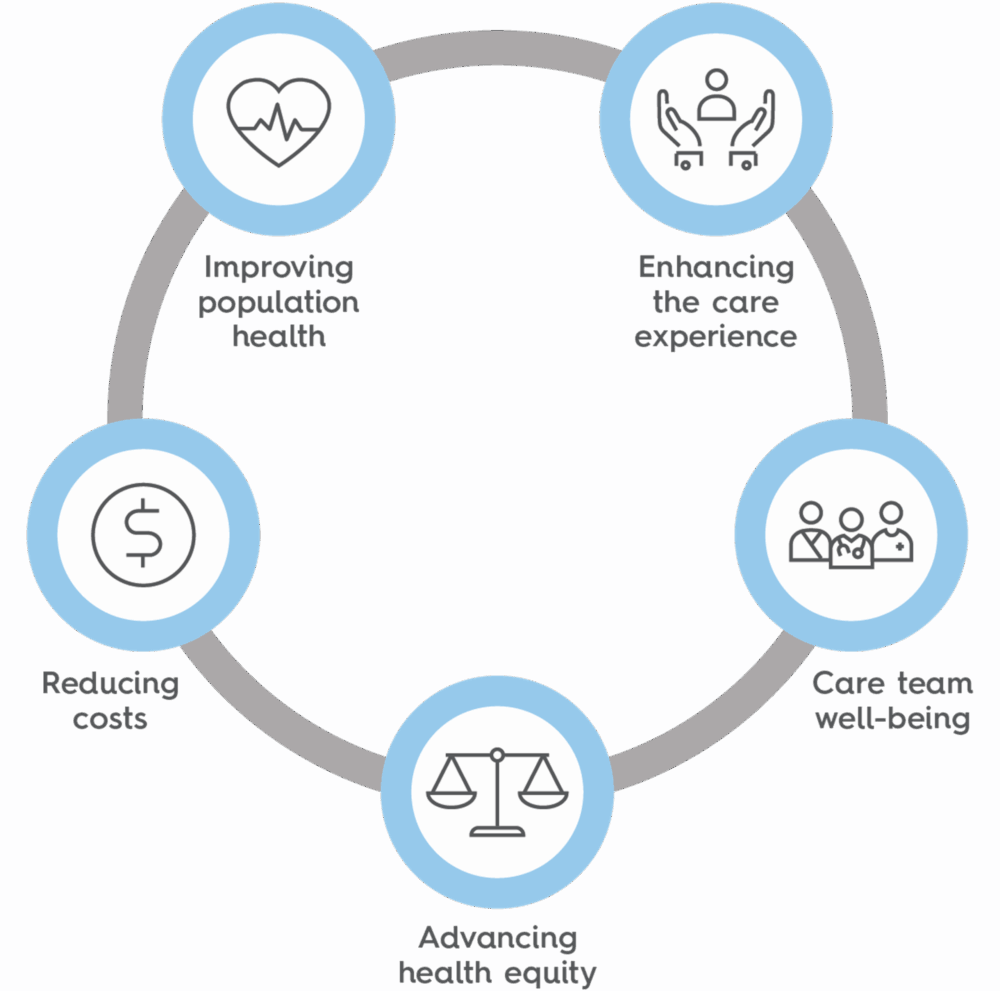
This year, our Commissioned Services Reporting Portal (CSRP) and Performance Management Framework continued to support ongoing improvement across the sector. This included a greater focus on measurement and evaluation to ensure our commissioned services are efficient and effective and we are delivering value through improved population health, enhanced patient experience, reduced costs, improved provider experience, and health equity.
We launched new reports in the CSRP for alcohol and other drugs and Integrated Chronic Disease Care services, offering comprehensive data visualisations, user-friendly interfaces and customisable views to enhance data analysis capabilities and support the delivery of high-quality services.
In our commitment to diversity and inclusion we developed Cultural Competency, Equity and Inclusion Commissioning Guidelines, providing essential information to enable commissioned service providers to advance along the cultural continuum toward delivering culturally safe, equitable and inclusive services. These guidelines are shaping changes in the commissioning process, clarifying expectations and enhancing measurement, evaluation and reporting of cultural competency, equity, inclusion and safety. This year we established a process to evaluate inclusive and culturally competent service providers during tender evaluation.
Established to ensure ongoing and direct engagement with our commissioned service provider organisations, our Service Provider Panel provided valuable feedback and insights over the past year informing and influencing discussions around multidisciplinary team care, WAPHA’s Commissioning for Better Health program and mental health service provision, including opportunities and barriers to service delivery.
Commissioning in action
WAPHA invested more than $233 million and funded 290 services to improve the health and wellbeing of Western Australians in 2024-2025. Here are a few highlights:
This year 27,655 clients received mental health support from commissioned services, through 199,880 occasions of service.
We launched the Depression starts small, get help before it grows campaign to raise awareness of the early symptoms of depression and promote help seeking behaviours. The campaign garnered 1.3 million views in the two months it was live. This campaign is part our GP-centric depression management program approach which aims to help improve the care of people with depression and prevent suicidal behaviour.
Over the last year, we supported more than 570 health professionals to upskill in managing and treating depression and suicidality and funded 185 community training courses in suicide prevention.
We established WA’s fifth Medicare Mental Health Centre in Northam, offering free advice, support and, if needed, assessment and treatment for people with stress, anxiety and other mental health challenges. Over the last year, 2,573 people visited one of WA’s five Medicare Mental Health Centres, with 16,268 sessions of support delivered, including mental health assessments, psychological therapy, peer support, group programs, and service navigation to connect people with ongoing care.
The state-wide Medicare Mental Health phone service received 6,596 phone calls, offering free confidential assessment and referral to appropriate supports – including Medicare Mental Health Centres, digital mental health supports, and public and private local community support services -for anyone seeking help for their mental and emotional wellbeing and/or wanting to support a patient, or someone they care about.
This year 2,326 Aboriginal clients received support from commissioned mental health services through 19,500 occasions of service, including assessments, therapy sessions, referrals, follow-ups, and other forms of support.
Twelve months in, digital mental health service MOST received 1,542 referrals with 797 young people going on to take up the service, adding effective, evidence-based digital support to the youth mental health system right across WA. The service is a digital mental health service for young people aged 12-25 providing online therapy content, tools and activities. It also provides access to connect with people online including other young people (on a safe, moderated social network), clinicians and career consultants.
In 2024-2025 3,399 clients received support from commissioned alcohol and other drugs services through 21,375 occasions of service. Support included screening and assessment, counselling and therapeutic interventions, harm reduction support, referral and care coordination and follow-up and monitoring.
We established WA’s eighth Medicare Urgent Care Clinic (MUCC) in Gosnells, providing treatment for urgent, but not life-threatening, illnesses and injuries requiring same day assessment for people who may otherwise have visited an emergency department. Over the last year, there have been 118,534 presentations across WA’s MUCCs, and 48 per cent of patients would have otherwise gone to an emergency department. We collaborated with Moodijit Koort and Arche Health to provide guidance and support to MUCCs on how to make their facilities culturally safe and welcoming for Aboriginal patients.
Through GP after hours support in residential aged care homes in Geraldton, 394 telehealth consultations and 124 face-to-face visits were provided. The service allows residents to be safely managed in their own care settings and prevents unnecessary transfers to hospital.
Through integrated models of care and strategic partnerships, WAPHA is working to enhance coordination across the primary health care system, reducing duplication, improving efficiency and ensuring resources are directed where they are needed most.


17
nurse practitioners placed across 14 general practices as part of the Nurse Practitioner and Team-Based Primary Care Pilot. Over an eight-month period, patients spent a total of 2,671 hours with a nurse practitioner to diagnose and treat illnesses, manage chronic conditions, and focus on preventative care, at no cost to them.
5,516
Aboriginal clients accessed Integrated Team Care through 68,490 occasions of service, including care coordination, health system navigation and access to services such as allied health.

2,148
clients accessed care finders, a service supporting vulnerable older people to navigate the aged care system, with 14,524 care finders services delivered.

678
general practices and over 290,000 patients in WA registered for MyMedicare, designed to provide continuity of care through formalising the relationship between patients, their general practice, GP and primary care teams.
20
general practices across WA integrated non-dispensing pharmacists into their teams, undertaking 15,863 activities delivering clinical pharmacy and education services to patients and practice staff.
363
patients were supported across WA’s two pelvic pain and endometriosis clinics in Murdoch and Albany, ensuring patients receive holistic care under one roof, reducing fragmentation and improving continuity of care.
Collaboration key to one health system
The pursuit of a high-performing, equitable and sustainable health system hinges on the strength of collaboration between state and federal health and mental health agencies and the Aboriginal Community Controlled sector. This collaboration is not just strategic but is essential for addressing the complex health needs of the diverse population in WA maximising the impact of our individual resources.
This year we finalised a partnership with the Australian Government Department of Health, Disability and Ageing (DHDA), the WA Department of Health and the Aboriginal Health Council of WA to formalise our shared commitment to enhancing primary health care and creating a unified health system in Western Australia. Collaboration between WAPHA and key federal and state health agencies is critical to maximising the impact of our respective resources.
This formalised commitment responds to the National Health Reform Agreement and Closing the Gap priorities and is designed to:
- Foster joint planning and shared accountability for health outcomes.
- Enable collaborative commissioning of services that are responsive to local needs.
- Support a ‘one health system’ mindset that transcends traditional structural boundaries.
Multidisciplinary teams strengthening primary health care
Multidisciplinary care teams operating within general practice are increasingly demonstrating their ability to support busy GPs and increase patient access to affordable, appropriate and coordinated primary care.
Over 60 practices have been involved in WAPHA’s pilots and programs aimed at strengthening primary care, improving access and advancing health equity in WA.
This year, in partnership with the WA Department of Health, WAPHA placed 17 nurse practitioners across 14 general practices in metropolitan and country areas, as part of the Nurse Practitioner and Team-based Primary Care Pilot. This initiative strengths multidisciplinary team-based care and the delivery of high-quality connected care for patients, especially for under-served populations. Over an eight-month period, patients spent a total of 2,671 hours with a nurse practitioner to diagnose and treat illnesses, manage chronic conditions, and focus on preventative care, at no cost to them.
Twenty general practices across WA integrated non-dispensing pharmacists into their teams, supporting improved patient outcomes and quality use of medications. As part of the care team, non-dispensing pharmacists deliver clinical pharmacy and education services to patients and practice staff through a coordinated, collaborative and integrated approach. Over the last year, 15,863 activities were undertaken by non-dispensing pharmacists in general practice.
Our Chronic Heart Failure Pilot entered its second phase, providing participating practices with an on-site, non-dispensing pharmacist for 15 hours a week over a 12-month period. The pilot is a general practice-led, multidisciplinary initiative aimed at improving outcomes for patients with chronic heart failure through better care coordination, education and system integration. Nannup Medical Practice’s team, led by the non-dispensing pharmacist, forged an innovative partnership with Advara HeartCare to provide travelling cardiovascular services, including free echocardiograms, which are helping to improve the early detection and management of chronic heart failure among their patients and ultimately helping to avoid hospitalisations.
The Optimising Primary Care Coordination for People Living in Residential Aged Care Homes project, funded through the National Partnership Agreement, has wrapped up its first phase with encouraging results. This work aims to build internal aged care capacity to deliver quality primary, end-of-life and palliative care and to reduce GPs’ administrative tasks. Phase one resulted in:
- Increased numbers of family meetings facilitated across all eight participating residential aged care homes and an improved screening process to identify patient complexity. This led to a reduced, but more targeted, approach to identifying the need for case conferencing, therefore supporting the work of GPs.
- Improved utilisation of specialist palliative care services, resulting in a more targeted approach to referrals to the Metropolitan Palliative Care Consultancy Service.
- Increased uptake of advance care planning.
- Increased completion rates of the Residential Goals of Care.
- Reduced numbers of residents transferred to the emergency department.
Over the past year, 2,148 clients accessed care finders, a service supporting vulnerable older people to navigate the aged care system, with 14,524 care finders services delivered. The network of care finders supports improved integration between the health, aged care and other systems at the local level.
WAPHA has played a central role in the rollout of MyMedicare across WA through strategic planning, operational coordination and practice engagement and support. To date 678 general practices and over 290,000 patients in WA registered for MyMedicare, designed to provide continuity of care through formalising the relationship between patients, their general practice, general practitioner and primary care teams.
This year 363 patients were supported across WA’s two pelvic pain and endometriosis clinics in Murdoch and Albany. Clinics are structured around GP-led teams that include nurse practitioners, pelvic physiotherapists, dietitians and allied health professionals. This ensures that patients receive holistic care under one roof, reducing fragmentation and improving continuity of care.
Over the past year 5,516 Aboriginal clients accessed Integrated Team Care through 68,490 occasions of service, including care coordination, health system navigation and access to services such as allied health. Care coordination made up 47,610 services clients received. This service supports Aboriginal people with chronic conditions to access the health care they need.
This year we launched our Chronic Conditions Care Strategy 2025-2027 to guide models of care and commissioning priorities for people with complex and chronic health needs. This strategy emphasises integrated care and aligns with national health priorities.
Stakeholder engagement is everyone’s business at WAPHA and building a strong culture of engagement practice, underpinned by our Framework, enables us to engage with our stakeholders consistently, inclusively and effectively. In our ongoing commitment to authentic partnerships and purposeful engagement to progress our strategic priorities, this year we refreshed our Stakeholder Engagement Framework.
A joint initiative between WAPHA, Rural Health West and the Royal Australian College of General Practitioners WA, the GP Advisory Panel is a unique approach to engaging directly with general practitioners on important topics that has strengthened the influence of general practice in planning, design and policy setting for primary health care. Over the past year, the panel has provided valuable feedback and insights around Rural Health West’s Inaugural State Budget Submission, mandatory health assessments as part of Firearms Act reform, increased GP training placements and impact on practices, and mechanisms for the partner agencies to gather feedback from GPs.

WAPHA is committed to strengthening the foundations of primary health care in WA through a sustained focus on capacity building.

$9.1 million
investment targeting GPs including individual support, digital integration and enhanced practice support programs.
526
WA general practices using Primary Sense, a clinical decision support and data extraction tool.

Tailored support
provided to more than 260 general practices across WA, including more than 6,500 quality improvement activities.

1,174
participants in our online and face-to-face training events to build capacity in primary care.

49,366
contacts to our no cost Practice Assist service, providing advice, resources and education to help strengthen general practice across WA.

368, 500 views
Our Clinician Assist WA website received over 368,500 views, providing GPs and other health professionals with guidance for assessing, managing and referring patients.
Guided by the Quintuple Aim and a vision of better health, together, our approach centres on supporting a sustainable, skilled and responsive primary care workforce.
This includes investing in workforce planning, training pathways, digital enablement, and integrated service models that empower general practice and allied health providers to deliver high-quality, person-centred care.
Supporting quality improvement and building capacity in primary health care
During 2024-2025 WAPHA invested $9.1 million in supporting GPs with digital integration and enhanced practice support programs. This included quality improvement (QI) activities and support with the use of digital health tools such as Telehealth, My Health Record, ePrescribing and secure messaging to improve the digital capability, data security, practice sustainability and patient outcomes.
Over the last year our QI team provided tailored support to more than 260 general practices across WA. Collectively, the team undertook over 6,500 QI engagement activities, with a focus on strengthening chronic disease management, preventative health and practice outcomes aligned to the Quintuple Aim.
Our QI coaches partnered with practices to embed continuous quality improvement approaches, support the integration of multidisciplinary team members, and co-design QI activities aimed at improving patient outcomes. The team made significant progress supporting practices through RACGP accreditation and partnered with Cancer Council WA to co-design CPD-accredited QI activities focused on improving cancer screening rates in general practice.
Our no cost Practice Assist service continued to provide advice, resources and education to help strengthen general practice across WA, with 49,366 contacts over the last year and over 100,800 individual visitors to the Practice Assist website.
This year, we ran 80 educational events to build capacity in primary care, with more than 1,170 people participating in our online and face-to-face training events.
We launched Clinician Assist WA, a secure, locally managed website to support GPs and health professionals with clinical and referral guidance, replacing HealthPathways WA and improving access to trusted resources. Clinician Assist WA ensures that GPs and other health professionals have the needed resources for assessing, managing and referring patients across WA, all at no cost. Over the last year 46 per cent of GPs in WA registered for Clinician Assist WA, and there were 368,500 page views across the site.
To improve cultural safety in care for Aboriginal people living with overweight and obesity, we launched two videos for primary health care practitioners focused on enhancing communication and fostering trust through social yarning and management yarning. Part of WAPHA’s SHAPE website, Yarning about weight: Building trust through social yarning and Yarning about weight: Setting goals and supporting change through management yarning offer practical techniques to create a more supportive and culturally safe environment for Aboriginal people to discuss their weight-related health concerns.
Also launched this year, our Aboriginal Weight Management eLearning modules promote culturally safe practices by fostering understanding of Aboriginal community values, social determinants of health and the impact of weight stigma.
We provided free online Aboriginal cultural awareness training to general practices, with 156 GPs and practice staff completing the course this year.
Nine general practices took part in the Palliative Care Champions project, building advance care planning and palliative care capacity and capability in general practice. There was a 62.5 per cent increase in the number of advance care plans completed across those practices.
Leveraging digital technology in health care
WAPHA is focused on leveraging technology as an enabler in health care for consumers, clinicians and service providers. Our leadership of national digital initiatives such as Primary Health Insights and Primary Sense helps to improve population health outcomes, nationally as well as locally.
Primary Sense, a clinical decision support tool that helps health care practitioners give patients the right care at the right time, is used by 526 WA general practices, processing over 4 million patient records.
Over the last year Primary Sense has advanced primary care analytics across WA, facilitating timely, data-driven decision-making. It has provided essential support to general practices through real-time medication safety alerts and patient-specific care prompts, enabling clinicians to identify high-risk patients and intervene early. Each month, Primary Sense triggers 19,000 care prompts and 1,500 medication safety alerts.
Primary Sense has been instrumental in supporting primary health care programs within general practice. It has played an important role in program planning, practice selections and evidence-based quality improvement initiatives, such as the Chronic Heart Failure Program, Greater Choices for At Home Palliative Care Program, Immunisation Program and Cancer Screening Program.
Supporting workforce planning
Our GP Workforce Planning and Prioritisation Summit brought together more than 60 GPs and key stakeholders from across WA to engage in dynamic discussions and share insights and strategies to address the challenges with GP workforce shortages.
As the provider of the GP workforce planning and prioritisation activity in WA, this year we consulted with more than 792 individual stakeholders to develop independent analysis and advice to the Australian Government on GP training placements to meet current and future GP workforce needs. Recommendations guide the two GP colleges, the Royal Australian College of General Practitioners and the Australian College of Rural and Remote Medicine, in their selection and placement allocation of GP Registrars in WA.
WAPHA’s commitment to being a capable organisation enables us to deliver on our three core functions – commissioning, capacity building and coordination.
This year, we have continued our efforts to strengthen WAPHA’s organisational capability through investing in our people, our systems and our culture.


Information security
Achieved ISO 27001:2022 Certification

QIC accreditation
Achieved QIC Health and Community Services Standards accreditation

Cultural awareness
100% of employees completed cultural awareness and LGBTIQA+ learning modules

Reconciliation Action Plan
RAP 2025-2027 formally endorsed by Reconciliation Australia

Rainbow Tick
Achieved Rainbow Tick accreditation mid-cycle assessment

Reducing greenhouse gases
100% of WAPHA’s metropolitan Perth pool cars hybrid
Cultural competency and diversity
Cultural competency, diversity and inclusion are key to achieving health equity across WA and this starts from within. All WAPHA people have completed cultural awareness and LGBTIQA+ equity and inclusion training, and this year, 15 people completed an Aboriginal cultural immersion program with an Aboriginal Elder on Country.
This year, WAPHA was re-accredited against Rainbow Tick Standards, strengthening the value we place on supporting, respecting and celebrating the individual differences of our staff and the broader WA community. We also developed WAPHA’s internal Gender Affirmation Policy to provide guidance to employees who are affirming their gender and to people leaders on how to best support employees throughout the process.
We developed and launched our Innovate Reconciliation Action Plan 2025-2027 as part of our commitment to ongoing, meaningful and respectful reconciliation, underpinned by genuine collaboration. We were also successful in gaining endorsement for neurodivergence to be included as part of WAPHA’s Diversity, Equity and Inclusion strategy.
Investment in our people
WAPHA maintains a strong commitment to investing in the people that make our organisation strong. This is demonstrated through growth and learning opportunities for WAPHA people, leadership training, peer-to-peer recognition and dedication to mental health support.
Through the Evolve program, we approved 68 learning requests to provide financial support for employees pursuing external learning for their professional development. Other key elements of support included:
- Leader learnings held at all levels, covering topics like change management, innovation and driving peak performance
- A refreshed onboarding program and content to streamline the process for new employees
- Development of our WAPHA Leadership Strategy, scheduled for launch in 2025-2026
- Development and launch of a new talent assessment tool
- Development and launch of a new performance appraisal tool
- Seven Lunch&Learn events with external providers, covering topics like menopause, neurodiversity and financial wellbeing.
Employee experience and wellbeing are vital to providing the best experience for WAPHA people. This year, we launched a staff recognition platform, Applaud, which has garnered 186 peer-to-peer shoutouts. In addition, we launched WAPHA’s new volunteering program, allowing employees to use paid leave to volunteer with value-aligned organisations. The program promotes community connection, strengthening ties in regional communities and enhancing employee wellbeing. Our Employee Experience Champions promoted and organised cultural events, including NAIDOC Week, Harmony Week, National Sorry Day and National Reconciliation Week.
WAPHA’s Wellbeing Advocates have also been hard at work this year. The team raised awareness of mental health with the 2025 Push Up Challenge – 21 employees participated, completing a total of 36,675 pushups. We also celebrated RUOK? Day and WA Mental Health Week by providing valuable resources, activities and learnings to our people. Wellbeing Advocates also engaged across WAPHA by promoting the Employee Assistance Program, publishing monthly wellbeing blog posts and highlighting other wellbeing initiatives.
Information security and governance
A key organisational highlight this year was achieving ISO 27001:2022 Certification, reflecting WAPHA’s unwavering commitment to the highest standards of information security management. This certification means that WAPHA has a system in place to manage risks to data security and that we are committed to following best practices and principles.
To demonstrate a strong commitment to good governance, community engagement and delivery of services, WAPHA achieved QIC Health and Community Services Standards accreditation. There were numerous strengths identified in our assessment, including leadership, culture, environmental sustainability and robust frameworks.
This year we established an Emergency Response Team (ERT), a leadership team that can be called upon to provide timely advice and guidance in the event of significant risks or incidents. The ERT is a key part of WAPHA’s Business Continuity Framework, ensuring that incidents are managed effectively and that impacts to WAPHA’s business are minimal.
Sustainability
At WAPHA, capability starts with sustainability. WAPHA is the first PHN to track its carbon footprint through Power Business Intelligence software. WAPHA’s carbon emissions dashboard focuses on office energy, waste, transportation and IT/digital emissions across each office.
The progress in sustainability across WAPHA has been significant. WAPHA’s Subiaco tenancy attained accreditation under the NABERS 5-star building performance rating for 2024-2025. The Subiaco office also achieved the First Ranking Tenancy Award for recording the lowest energy kilowatt usage based on net lettable area for the Subiaco building in 2025.
During 2024-2025, WAPHA recorded a total of 149.2 mtCo2 emissions. This sets the strategic metric indicator for WAPHA’s carbon emissions and gives us a benchmark by which to measure our progress as we continue carbon emission tracking across the key focus areas at WAPHA’s eight offices. Recycling is also a key component of WAPHA’s sustainability efforts as we recycle everything from batteries to lighting tubes, and recycled paper, stationery and cleaning products are used across the organisation.
To further reduce greenhouse gases, WAPHA’s metropolitan pool cars are now 100 per cent hybrid. There are plans to introduce 4×4 hybrid vehicles to WAPHA’s regional fleet, and where practical, to introduce the GoGet Car Sharing arrangement scheme to further lower emissions and reduce costs. Sustainability efforts are ongoing, and as new ideas emerge to reduce WAPHA’s carbon footprint, they will be considered and implemented.
Financial Snapshot
Find out how our funding has been allocated over the past year.
