Primary health care providers are critical in recognising family,
domestic and sexual violence, creating safety for disclosure
and activating support services.
Need help? Quick exit
Family, domestic and sexual violence is a significant public health issue across Australia, with inter-generational consequences for physical and mental health.
As part of the Australian Government’s commitment to the National Plan to End Violence against Women and Children 2022-32, WA Primary Health Alliance has been successful in its application for two grants to support an effective primary health care response to FDSV.
Two pilot programs will be conducted over three years in locations selected by the Australian Minister for Health and Aged Care.
Working with local stakeholders, WAPHA will adapt a national model for integrating general practice care with the broader service response. This project will be underpinned by a partnership approach that learns from lived experience and established organisations with expertise in the FDSV service response.
In Perth South PHN, the program will focus on supporting the primary care sector response, and in Country WA PHN, the pilot will focus on supporting recovery using a new model of trauma informed care.
This will involve working with key stakeholders like FDSV service providers, peak advisory bodies and people with lived experience to enhance the capability of the general practice team to identify patients and families being affected by FDSV connect them to vital FDSV services.
Quick links:
Project Activity Lead: Carolyn Donovan
carolyn.donovan@wapha.org.au
08 6272 9543
WA Primary Health Alliance acknowledges the individual and collective expertise of people with a lived or living experience of family and domestic sexual violence.

Need help?
If you find yourself in an emergency, or at immediate risk of harm to yourself or others, contact emergency services on 000.
1800RESPECT 1800 737 732 is a 24-hour national sexual assault, family and domestic violence counselling line for any Australian who has experienced, or is at risk of, family and domestic violence and/or sexual assault.
Individuals can also access local support services and search the internet using Daisy, a free app developed by 1800RESPECT that protects user privacy.
Click to expand
The Australian Government is funding our Country WA Primary Health Network to develop trauma-informed recovery care services for victim-survivors of family, domestic and sexual violence. The pilot location, Geraldton, was selected after a thorough decision-making process that considered both demand and supply requirements.
Two complimentary service types will be commissioned in Geraldton by WA Primary Health Alliance (WAPHA) during 2024, providing case management and psychological therapies for up to two years per client. The pilot aims to promote sustained recovery and address trauma-related mental health conditions for victim-survivors of FDSV.
WAPHA will work with local stakeholders to maximise the outcomes of the pilot and establish a scalable model for long-term trauma-informed mental health care. Interested organisations in Geraldton can subscribe to receive WAPHA tender notifications and express interest in delivering one or both services.
Submissions have now opened for organisations interested in delivering the Family, Domestic and Sexual Violence (FDSV) Primary Care Integration Service in the cities of Armadale, Gosnells and Canning.
This service aims to improve the effectiveness of the primary care response to FDSV and integrate this into the broader local support system. It will support primary care providers to enhance their skills and confidence, create safe environments for disclosure and work collaboratively with specialist FDSV providers to improve care pathways. As part of the national Supporting Primary Care FDSV PHN pilot, the service will also support training, innovation, integration, and evaluation activities coordinated by WA Primary Health Alliance in these cities.
To achieve the improvements outlined above, the successful contractor will be required to establish and embed a part-time social work service that supports a whole-of-practice response within a minimum of six general practices. The social workers will also provide a referral service for other local general practices.
Find out more information apply here
On Thursday, 21 March, WA Primary Health Alliance launched the Enhancing Primary Care Response to Family, Domestic, and Sexual Violence (FDSV) pilot project. The breakfast, held at the Gosnells Golf Club, drew a good turnout from health care practices across the targeted Gosnells, Armadale, and Canning local government areas.
The launch event featured Dr Anna Chaney, a GP with extensive experience supporting patients impacted by violence and abuse. Dr Chaney provided helpful perspectives on the role of the GP and the value of working as a team, both within the practice and with local services. Carolyn Donovan, manager of the new South East FDV Healing Service in Armadale, discussed the comprehensive range of services that will be available at the hub, emphasising the potential for fostering collaboration between primary healthcare practices and support services. The discussion that followed amongst attendees demonstrated that the resources offered by the pilot program are both needed and welcomed.
Rosie Logie, the activity lead for the pilot project, explained the project’s origins, its early successes, and the benefits it now offers to practices in Perth’s south-east metro corridor. Among the project’s benefits is the provision of a collocated FDSV social worker, supporting practices to recognise, respond to and refer individuals impacted by FDSV. Additionally, a comprehensive training plan is being developed, that will provide CPD points to attendees.
Expressions of interest to participate in the project are now being accepted until 31 May 2024. To register your practice team’s interest or if you have any queries, please contact FDSV@wapha.org.auto to start the discussion of how the project can benefit your practice.
A number of new FDSV resources have been recently made available by the Australian Government.
- Australian Government Department of Health, Disability and Ageing – FDSV topic page (public facing)
- Australian Institute of Health and Welfare FDSV website
- Australian Bureau of Statistics – 21/22 statistics on partner violence
-
You can access these and other key resources in the FDSV State, national, and global policy context section below
Thankyou to those who have reached out to offer expertise following October’s stakeholder briefing.
As you can appreciate, these Pilots are complex and multifactorial, and the insights stakeholders have provided have been extremely useful.
Perth South PHN Pilot: South-east Metro – early intervention domain
The tender for the FDSV Local Link service will now open early 2024, with more details to follow.
Country WA PHN Pilot – recovery domain
The Supporting Recovery from FDSV Pilot requires WAPHA to consider multiple data sources to develop a comprehensive understanding of need, map the availability of existing services and assess risk to determine the location/s in which the Pilot is most likely to succeed.
Given the need to focus on recovery and healing, the selected location/s will need to be supported by a level of stability and safety within the community.
While acknowledging FDSV is new territory for PHNs, the combination of our strong partnerships, state-wide structure and access to comprehensive data sources means we are well placed to select location/s that will provide optimum conditions to run the Pilot and, in turn, deliver the best outcomes for the community.
WA Primary Health Alliance will ensure to keep you informed of the outcomes of our assessment.
The RACGP’s Lunch & Learn Series is a new knowledge-sharing network created to help frontline primary care professionals develop skills and confidence in responding to family violence.
You’ll be learning alongside other primary care professionals keen to make a difference to women and children.
Held on the 3rd Friday of every month, Lunch and Learn provides an excellent opportunity to gain insights and support in managing family violence.
This is a complex area of practice and it’s vital that we learn from one another’s lived experience of trying to support those affected.
Session dates:
Each Lunch & Learn session involves:
- Three panel members
- A presentation on a different aspect of family violence
- De-identified case presentations (submit your own case too)
- Q&A / discussion time.
We encourage you to submit a de-identified case for discussion – this is real-world training where practitioners are encouraged to share challenges and gain insights and ideas from professional peers walking the same path.
You can come to all meetings or attend as per your availability
You only need to register once to receive all zoom meeting links
30 Oct 2023
The Attorney-General’s Department, in partnership with Sate and Territory Governments, has released National Principles to Address Coercive Control In Family and Domestic Violence (National Principles). Available on the Australian Attorney -Generals Department website, the National Principles are supported by a range of fact sheets, videos and other resources to support healthcare practitioners recognise and respond to coercive control.
23 Aug 2023
As part of the Australian Government’s commitment to the National Plan to End Violence against Women and Children 2022-32, WA Primary Health Alliance (WAPHA) has been awarded two grants to support an effective primary health care response to family, domestic and sexual violence.
24 Aug 2023
Read the media release from The Hon Mark Butler MP Minister for Health and Aged Care.
The national PHN Family, Domestic and Sexual Violence Pilot is an expansion of a model developed by Brisbane South PHN that builds on existing pilots that are being expanded in:
- Brisbane South PHN
- Nepean Blue Mountains PHN
- Hunter New England and Central Coast PHN
- North West Melbourne PHN
A range of interests were represented in the design process, including Aboriginal communities and women with lived experience. An independent evaluation by the Sax Institute has recently been published and supports the expansion of the program.
The integrated response model comprises six influencing activities that support primary care to take up a defined role in the systemic response to domestic and family violence.
The first grant, Supporting the Primary Care Response to FDSV pilot relates to the Early Intervention domain of the National Plan with an aim to facilitate an improved, integrated primary care response to FDSV in the Armadale region and surrounds, in collaboration with the State Government’s new Family and Domestic Violence One-Stop hub in Armadale. WAPHA will commission a ‘system integrator’ to support general practices, delivering workforce capacity building activities and facilitating innovation to overcome barriers to integrated patient care.
The second grant, Supporting Recovery from FDSV pilot will be implemented in one or more regions of our Country WA PHN. This pilot relates to the Recovery and Healing domain of the National Plan. A draft service model has been developed by a national expert reference group and incorporates a small care team and long-term, trauma-informed therapies for up to two years per individual. The service must be embedded within an existing service.
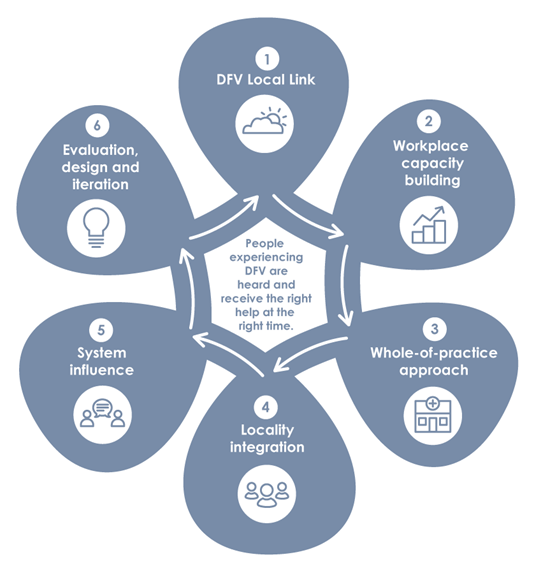
The integrated response model comprises six influencing activities that support primary care to take up a defined role in the systemic response to domestic and family violence.
- Path to Safety: WA’s Strategy to reduce family and domestic violence
- WA Aboriginal Family Safety Strategy
- WA Sexual Violence Prevention and Response Strategy (in development)
National:
- National Plan to End Violence Against Women and Children 2022-32
- Change the Story – national framework for prevention
- Australian Government Department of Health, Disability and Ageing – FDSV topic page (public facing)
- Australian Institute of Health and Welfare FDSV website
- Australian Bureau of Statistics – 21/22 statistics on partner violence
Global:
It is estimated that on average, a GP may see up to five women and/or children a week who are experiencing the impact of FDSV, and many of these will not be receiving or seeking support directly for FDSV. It is important that GPs and all practice staff are equipped to “Recognise, Respond and Refer” in a safe and effective way.
Under the new National Plan, Primary Health Networks (PHNs) have been allocated a specific role, reflecting a recent policy recognition of the role of primary care in an effective, integrated response for people experiencing family, domestic and sexual violence (FDSV).
The two grant rounds under which WA Primary Health Alliance is funded were open only to PHNs.
Subject matter experts and key stakeholders consulted during the application phase were supportive of WAPHA’s proposed role in these pilot programs.
Throughout the project, WAPHA will maintain established central advisory relationships with the WA Department of Communities Office for Prevention of Family Violence and the Centre for Women’s Safety and Wellbeing.
Design workshops will be held with key stakeholders to inform the design of activities, and an action research approach will be adopted to incorporate learnings as we progress.

