Our 2023-24 Year in Review showcases key achievements over the past year as we work to deliver better health, together.

Message from our Board Chair Dr Richard Choong and CEO Learne Durrington
On reflection, this past year can be summed up in two words – collective impact. This can be seen in the integration, collaboration and innovation among our team, but also working alongside our commissioned service providers and primary health care professionals to deliver better health, together.
![]()





Our strategic priorities
Show leadership and commitment to health equity and embed equity in everything we do Commission integrated primary health care services in a planned and targeted way
Continuously improve practice in primary health care Support a high-quality primary health sector that is embedded in the WA health system Lead the delivery and support of secure digitally enabled health care with partners locally and nationally Operate a fit for purpose organisation
![]()
Show leadership and commitment to health equity and embed equity in everything we do
To inform our Multicultural Competency and Capability Framework, we consulted with commissioned service providers, GPs, multicultural community members and our staff. Over 80 people shared their experiences of primary health care and opportunities to improve access for multicultural communities.
Read more
We launched our Multicultural Competency and Capability Framework, supporting us on a journey to better meet the primary health care needs of WA’s multicultural communities.
The new Framework provides a set of key principles for developing cultural competency, and standards with agreed actions to guide the design, development, implementation, and evaluation of cultural competency for WAPHA employees, commissioned service providers and primary care services.
Read more
We were re-accredited against Rainbow Tick Standards, strengthening the value we place on supporting, respecting and celebrating the individual differences of our people and the broader WA community. The re-accreditation process involved submission of over 80 pieces of evidence and a highly successful assessment week where over 45 of our people and stakeholders were consulted by the assessment team.
Read more
We released our Strategic Plan 2023-2026, setting out our priorities for the next three years and a path towards our vision of a more connected primary health care system, one that minimises barriers to accessing primary health care and ensures those with the greatest health needs are cared for as close to home as possible.
Read more
We launched our Suicide Prevention Strategy 2023-2025, outlining a systems-based approach to commissioning activities and services, targeting the primary mental health care sector and general practice, in particular.
We are targeting activities to those communities with the greatest identified need, based on comprehensive data collection and analysis, and, importantly, where all four components of the systems-based model can be applied.
Read more
WAPHA CEO Learne Durrington was appointed to the Strengthening Medicare Implementation and Oversight Committee, established to oversee primary care reform projects emanating from the Strengthening Medicare Taskforce Report.
As a 10-year program, Strengthening Medicare aims to fundamentally shift primary care to be more adaptive to population health needs and workforce needs.
Across Strengthening Medicare there are four key themes which are guiding the Committee:
- Improving access and increasing access to primary care.
- Voluntary patient registration.
- Improving and increasing primary care affordability and accessibility for people in disadvantaged locations and population groups.
- Strengthening after hours primary care.
WAPHA is closely assessing and interpreting progress of the Strengthening Medicare reform program and the implications for primary health care in WA. We understand the need to be agile and to align ourselves to reform agenda in a way that continues to build value in primary care, trust with stakeholders and good consumer outcomes.
We participated in a national consultation designed to assist the National Indigenous Australians Agency to understand alcohol and other drug workforce and data capacity building needs and inform future investment and enhancement of alcohol and other drug treatment services for Aboriginal people. As part of the consultation, WAPHA, along with other funders, shared alcohol and other drug KPIs and measures and sought to identify ways to reduce administrative burden on jointly commissioned service providers. Given WAPHA’s commitment to cultural competency, it was interesting to note that the consultation highlighted the importance of cultural and clinical supervision for provision of culturally safe services and the ongoing need to cultivate safe workplaces.
Commission integrated primary health care services in a planned and targeted way

We established four additional Medicare Mental Health Centres (formerly Head to Health services) in Gosnells, Mirrabooka, Armadale and Northam, offering free advice, support and, if needed, assessment and treatment for people with stress, anxiety and other mental health issues.
Read more
We launched Make the call on your mental health today, a campaign to raise awareness of the free mental health assessment and referral Head to Health phone service (1800 595 212), available statewide in WA. Since the campaign began, the average number of calls per month has increased by 182 per cent.
Read more
Two exciting digital mental health services, e-Friend and MOST were launched, reflecting our commitment to innovation in the commissioning of mental health services. Both services offer a more holistic and personalised experience for those who access them, offering online tools and support to help them get back on track in a way that suits them.
e-Friend provides lived experience peer support to help people with their mental health needs and is the first time a combined clinical-lived experience peer approach is being offered within an online clinical mental health service in Australia.
Read more
Building on lessons learned from the National Suicide Prevention Trial, we worked closely with communities, GPs and organisations across WA to tailor activities suited to the needs of their local communities. In just six months, these initiatives have supported around 1000 people from community members to clinicians, enabling them to improve care and recognise and respond to those in need of mental health assistance in their community.
Read more
We commissioned three state-wide needs assessments for the multicultural access, homelessness support and after-hours programs. The needs assessments included consultation and collaboration with internal and external stakeholders, including peak bodies, consumers and specialist support services, along with detailed data analysis to understand the after-hours, multicultural access and homelessness primary health care needs across WA and provide recommendations to support potential service commissioning.

Continuously improve practice in primary health care
We commissioned two endometriosis and pelvic pain clinics, in Albany and Perth respectively, to build the capacity of primary care to manage this condition and improve access to expert, multidisciplinary services.
The Garden Pelvic Pain Clinic in Murdoch, which has seen 184 women its first six months, provides patients with a personalised, evidence-based treatment plan through education, support and connection to a qualified multi-disciplinary team. Clinicians are focussed on the impact pain is having on a patient’s life and are led by treatment goals identified by patients, including improving quality of life, effective pain management, and improved daily functioning.
Read more
Using a grant received through WAPHA’s Organisational Strengthening and Development Grants Program, one of our commissioned service providers 360 Health + Community developed their Inclusion, Diversity and Wellbeing Framework, laying the foundation for inclusive program and service design. The Framework underpins the development of services, programs, policies and projects with a view to creating a sense of belonging and greater well-being for 360 Health + Community employees and clients from a range of communities.
Read more
A joint initiative between WAPHA, Rural Health West and the Royal Australian College of General Practitioners WA, the GP Advisory Panel is a unique approach to engaging directly with general practitioners on important topics has strengthened the influence of general practice in the planning, design and policy setting for primary health care.
Over the past year, the GP Advisory Panel has:
- Provided feedback on the Outpatient Reform Program.
- Offered insights for WAPHA’s Digital Health Strategy.
- Informed WAPHA’s Family Domestic and Sexual Violence pilot model.
- Participated in a special interest panel for the Head to Health Kids Hub.
- Explored the implications of MyMedicare for WA GPs.
- Contributed to the effectiveness review of the Practice Incentive Program and Workforce Incentives Program.
- Focused on workforce maldistribution, GP education needs, and general practice sustainability.
- Supported a positive and proactive general practice voice.
Read more
Established to ensure ongoing and direct engagement with our commissioned service provider organisations, our Service Provider Panel provided valuable feedback and insights over the past year informing and influencing discussions around indexation, primary health care workforce and the impacts of maldistribution and shortages, commissioning and procurement processes, WAPHA’s Digital Health Strategy and the implications of the Federal Budget 2024-25 for primary health care.
Insights provided by the Panel into procurement experiences (both with WAPHA and other organisations) and possible strategies we could implement are being used to improve our process and to create a space for open and honest discussions about procurement requirements, preferred suppliers and awarded tenders.
Read more
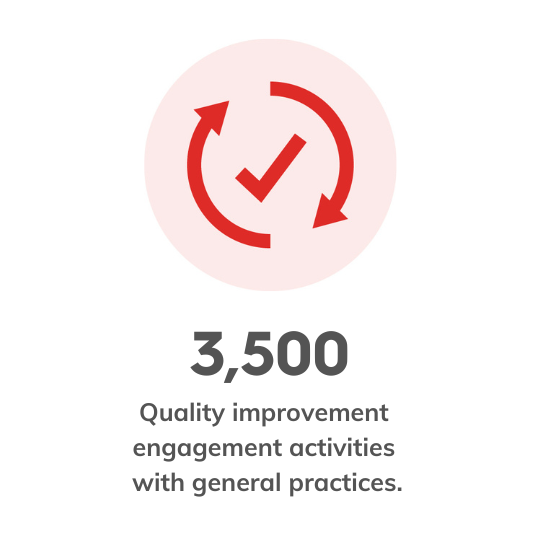
Our quality improvement team actively supported general practices in quality improvement (QI) activities across WA, including over 60 practices involved in commissioned programs, including the Nurse Practitioner and Team Based Care Pilot, the Non-Dispensing Pharmacist Program, the Early Intervention for Older Adults Program, the Chronic Heart Failure Program, and the Greater Choices for Palliative Care Program.
Beyond this, our QI coaches have undertaken over 3,500 engagement activities with general practices, delivering targeted support aimed at improving health outcomes in critical areas such as chronic disease management, preventative health, and the quintuple aim. By leveraging data and focusing on priority populations, we’ve empowered practice teams to implement co-designed, targeted QI initiatives based on their unique needs, patient demographics, and service delivery models, fostering continuous improvement in primary health care delivery.
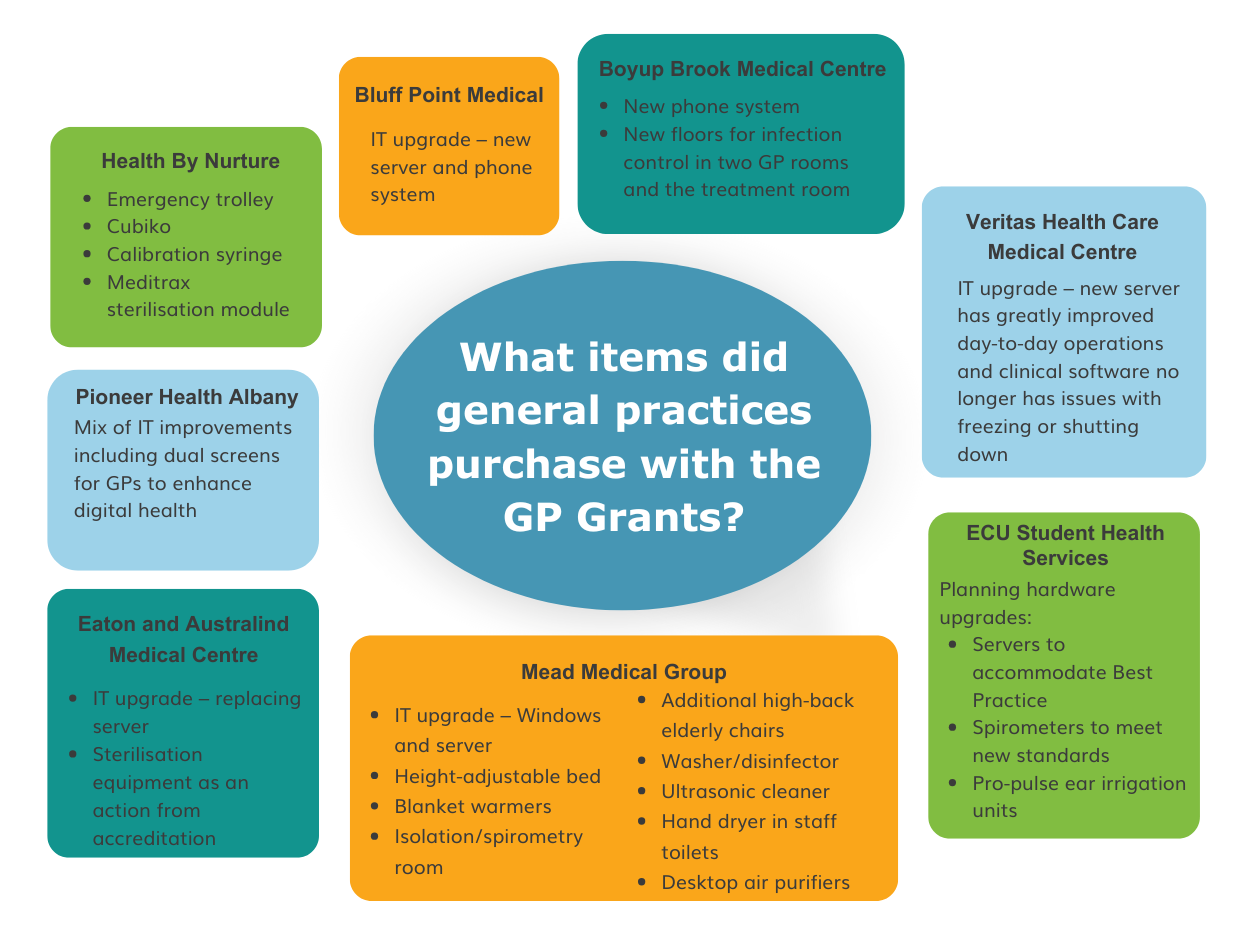
Over three months, WAPHA directed $17.5 million in Strengthening Medicare General Practice Grants to 653 general practices across WA. From upgrading IT systems allowing GPs to better deliver digital health, to isolation room fit outs and upskilling practice staff in data driven clinical care improvements, general practices across WA used Strengthening Medicare General Practice Grants to expand patient access and support safe, and accessible, quality primary care.
Support a high–quality primary health sector that is embedded in the WA health system

Overseeing the tender and commissioning process in WA, we supported the establishment of six Medicare Urgent Care Clinics (UCC) in Rockingham, Beeliar, Clarkson, Bunbury, Midland and Broome. The clinics offer treatment for urgent but not life-threatening illnesses and injuries requiring same day assessment for people who may otherwise have visited an emergency department.
Read more
WAPHA, the WA Department of Health and the five WA Health Service Providers signed up to a Memorandum of Understanding (MoU) outlining agreed principles of engagement, participation and working processes between all parties in achieving the intent of the Medicare UCCs. The MoU outlines how parties will work together to provide more sustainable health outcomes and to align with the systemwide reform intentions. The MoU also demonstrated the commitment to improving health care integration across the primary and acute health system in WA.
As the provider of the GP workforce planning and prioritisation activity in WA, we consulted with over 1006 individual stakeholders and 188 organisations to develop independent analysis and advice to the Australian Government on GP training placements to meet current and future GP workforce needs. Recommendations will guide the two GP colleges, the Royal Australian College of General Practitioners and the Australian College of Rural and Remote Medicine, in selection and placement allocation of GP Registrars in WA.
Read more
Building on the success of existing non-dispensing pharmacists in general practice services, we engaged the Pharmaceutical Society of Australia to provide non-dispensing pharmacists in general practices to support older people. Thirty general practices across WA have integrated non-dispensing pharmacists into their teams through this project, supporting improved patient outcomes.
Having pharmacists in general practice allows for a more coordinated and collaborative approach to care, which can lead to better access to integrated services for chronic conditions and improve health literacy around medications.
A strong evidence base for the continuation and scaling of this initiative is being developed and will inform ongoing improvement and model design.
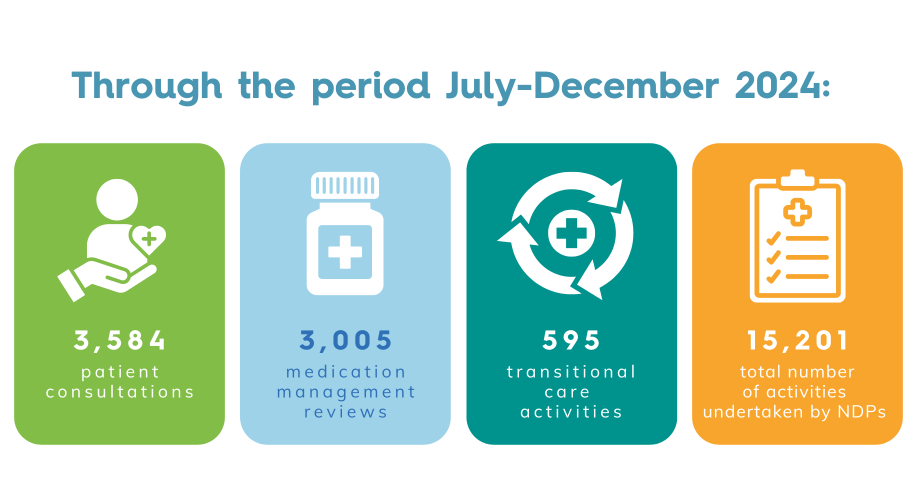
In collaboration with WA Department of Health, we successfully placed 16 nurse practitioners in 14 general practices as part of the Nurse Practitioner and Team-Based Primary Care Pilot.
The Pilot aims to enhance the availability and accessibility of comprehensive primary care to the WA community, including supporting the delivery of care to at-risk and under-served populations. Ongoing evaluation will inform the 18-month Pilot as well as being used to inform future primary care policy.
Two nurse practitioners have been placed in general practices in Albany, two in the Wheatbelt with the remaining twelve working in both general practices and Aboriginal Community Controlled Health Services within the Perth Metropolitan area.
Read more
We piloted a project to employ four dedicated case coordinators across eight residential aged care homes (RACH) in WA to improve palliative care and end-of-life support for older Australians.
Coordinators provide an important link between residents and their care teams with GPs involved in the residents’ care highlighting the improved efficiencies in identifying clinical priorities and addressing complex needs.
The project has had a significant impact in ensuring preferences at end-of-life are being documented and understood. Since the pilot began, 97 per cent of residents were able to have their preferred place of death recorded, and 95.7 per cent had their preferences met.
Read more
As part of the Chronic Heart Failure Pilot Project, we partnered with the WA branch of the Pharmaceutical Society of Australia to integrate non-dispensing pharmacists into the multidisciplinary teams within two general practices in Geraldton.
The non-dispensing pharmacists have added value through:
- Providing regular GP education sessions.
- Medication reconciliation and management.
- Medication dosage titration and adjustment.
- Supporting and enhancing chronic disease management plans.
- Providing education to patients with chronic heart failure.
Read more
Through WAPHA’s General Practice Emergency Response Team (GPERT) project, we developed a model that defines how general practice will engage in disaster prevention, preparedness, response and recovery in WA health response planning in disaster.
As part of the model design process, we consulted with over 400 stakeholders including health professionals, disaster professionals, established collaborative groups and district emergency management committees.
With the guidance of the WA GP Advisory Group, the developed GPERT model was endorsed and is progressing through approval channels to arrive at an authorised model.
Read more
Supporting Primary Care – Local Link Pilot
We established a pilot project to improve the effectiveness of the primary health care response to family, domestic and sexual violence (FDSV) and integrate this into the broader local support system. It will support primary health care providers to enhance their skills and confidence, create safe environments for disclosure and work collaboratively with specialist FDSV providers to improve care pathways. We now have five general practices within the Armadale, Gosnells and Canning regions who have committed to participating in the project.
Supporting Recovery Pilot – Country WA
We are commissioning trauma-informed recovery care services for victim-survivors of FDSV. The pilot location, Geraldton, was selected after a thorough decision-making process that considered both demand and supply requirements. Two complementary service types are being commissioned in Geraldton, providing case management and psychological therapies for up to two years per client. The pilot aims to promote sustained recovery and address trauma-related mental health conditions for victim-survivors of FDSV.
Read more

Lead the delivery and support of secure digitally enabled health care with partners locally and nationally
Since practice registration began in July 2023, we have supported general practice to understand the potential benefits of MyMedicare and contextualise information from Services Australia on how to complete the registration process before patients were invited to register
We have supported general practices to register for MyMedicare, providing information, resources and in some cases, assistance to enable practices to successfully complete their registration and to provide their patients with information on the benefits of the program.
Around 90 per cent of general practices in WA have registered for the MyMedicare program.
Read more
We commissioned telehealth technology provider Visionflex to deploy 180 telehealth carts to residential aged care homes (RACH) across WA, equipped with video camera capabilities, a digital stethoscope, pulse oximeter, blood pressure cuff and a state-of-the-art examination camera.
The carts improve the quality and accessibility of primary care services for residents, reduce the need for travel, limit unnecessary hospitalisations, and allow for early detection and treatment of chronic conditions.
Our dedicated digital health team travelled across the state to engage with general practices and RACHs, offering education and assistance and finding out first-hand how the telehealth carts care making a positive impact.
Read more
With a vision to improve delivery of health care innovations and enable new ways of working, we launched our 2024 -2026 Digital Health Strategy. The Strategy describes how we will lead the delivery and support of secure digitally enabled health care and drive the meaningful use of digital health to enhance the quality, efficiency and accessibility of care. Central to this is an interconnected health system where communications and data sharing between health care providers, key stakeholders and WAPHA are enhanced to improve the quality and availability of secure health data, insights and information.
Read more
WAPHA leads the operation and development of Primary Health Insights, the data and analytics storage platform used by 30 PHNs.
Since going live in late 2020, the PHI Services Team at WAPHA has worked with PHNs in expanding the use of the platform significantly beyond its original vision. In addition to its secure data storage and analytics capabilities, PHI now hosts a variety of applications and facilitates a number of technology development and data collaboration initiatives.
Over the past year, the PHI Services Team at WAPHA has successfully completed a number of projects aimed at enhancing PHNs’ capabilities to independently utilise the tools and solutions in PHI. With the growing importance of using data to drive decision making, this will support PHNs in achieving their objectives. Projects include the development and provision of position description templates that will help PHNs recruit skilled staff and help to align roles and responsibilities across PHNs, and a National Staff and Skills Directory of PHN staff working in the data analytics or data engineering field to foster peer collaboration and support nationally.
The team has also successfully deployed and trained all PHNs to use the Primary Health Operational and Commissioning Unified System (PHOCUS). Hosted within the secure PHI environment, PHOCUS is a new system used by all PHNs for performance reporting. It assists the Australian Government Department of Health and Aged Care in making data-driven decisions at a program and policy level. PHOCUS is now the source of all data for PHN Performance Management Reporting Framework and Medicare Urgent Care Clinic insights. The Team at WAPHA continues to work with the Department to enhance PHOCUS’s functionality and expand its scope to further datasets.
Led and operated by WAPHA, general practice clinical decision support and data extraction tool Primary Sense is now used by 12 PHNs and 7,800 GPs and nurses across Australia. It assists GPs in clinical decision making, both within the practice and in real-time during patient consultation.
From uncovering a stronger correlation between panic attacks and asthma to demonstrating how changes in COVID-19 infections relate to hospitalisation, Primary Sense is providing previously inaccessible health data and insights to PHNs and GPs.
Primary Sense has supported us to:
- Determine whether people with a serious mental health condition were ‘equally well’ and receiving adequate treatment for their physical health conditions compared to people without a mental health condition.
- Develop a methodology to use clinician diagnoses to calculate population prevalence rates for a range of conditions. This provides a geographically granular understanding of population health needs.
- Support primary health care programs in general practice, including program planning, practice selections and evidence-based quality improvement e.g. Chronic Heart Failure Program, Greater Choices for At Home Palliative Care Program, Healthy Weight Program, Community Physio Program and clinical care coordination for patients with schizophrenia.
- Provide the evidence base for the SHAPE healthy weight program’s quality improvement initiatives in general practice.
WAPHA is currently undertaking a proof-of-concept data linkage project between general practices and hospitals. This will enable the tracking of patient journeys between primary and hospital care, better understanding the relationship between primary and acute care and the impact of WAPHA’s activities.
Operate a fit for purpose organisation
Our stakeholder relationship management (SRM) system is a key strategic asset and critical to ensuring we can communicate and engage effectively with our stakeholders. Over the last twelve months we have made numerous enhancements to the functionality of the platform which will significantly improve reporting outcomes, and the implementation and adoption of revised user guides and processes. These include:
- Development of a comprehensive dashboard report for our workforce planning and prioritisation team enabling data capture to inform the bi-annual workforce needs and training capacity report.
- SRM inclusion as a business-critical training resource in WAPHA’s welcome program/onboarding, to be implemented in the second half of 2024.
- More than 11,500 general practice engagement activities recorded by our practice support team.
- 4,380 contact records and 1,959 organisation records created and/or updated.
We launched a new policy that underpins our position on climate change and commitment to reduce our carbon footprint in five key areas of focus – energy, transportation, waste, IT digital, and employee engagement. A reduction in carbon emissions in these areas aims to minimise our impact on the environment and address the issue of climate change.
Some of the key initiatives to support this work include:
- Implementation of over 25 new sustainability initiatives across WAPHA offices.
- Collation of sustainability data to track WAPHA’s overall carbon footprint in the five key focus areas.
- Attainment of a National Australian Built Environment Rating System 5-star accreditation certification for energy performance consumption at WAPHA Subiaco premises.
- Introduction of 100 per cent hybrid pool vehicles for WAPHA’s metro fleet.
- Creation of a strategic metric data set to track and monitor sustainability data for all WAPHA offices.

People and Culture
Creating meaningful employee experiences, encouraging continuous learning, and nurturing and developing leadership skills.
Financial Snapshot
Find out how our funding has been allocated over the past year.