We are taking on an enhanced role in supporting the health and wellbeing of older Australians.

As part of the Aged Care Program, we are designing, commissioning, and delivering activities to support access to primary care and aged care services for older Australians.
Many older Australians are now living longer and healthier lives, however there are many who lack appropriate access to primary care, opportunities for social interaction and economic engagement within their communities.
Funding under the Australian Government Aged Care Reform Package to Primary Health Networks (PHNs) is focused on initiatives with the overarching goal of delaying entry into residential aged care homes (RACHs) and reducing avoidable hospitalisations for older Australians.
The Final Report: Royal Commission into Aged Care Quality and Safety identified several areas that affect aged care residents and our health system, including limited access to GPs and allied health professionals in RACHs, difficulties accessing out of hours services and unnecessary hospital transfers.
To help us understand community needs, aged care system capacities and areas for investment, stakeholder consultations were undertaken throughout 2022. We will continue to build relationships and hear from the WA aged care sector, GPs through the care of the older person specialist interest panel, community members and state government departments.
The Australian Government has provided aged care and dementia activity funding guidance to support us to design, commission and deliver the following activities.
Click below to read more
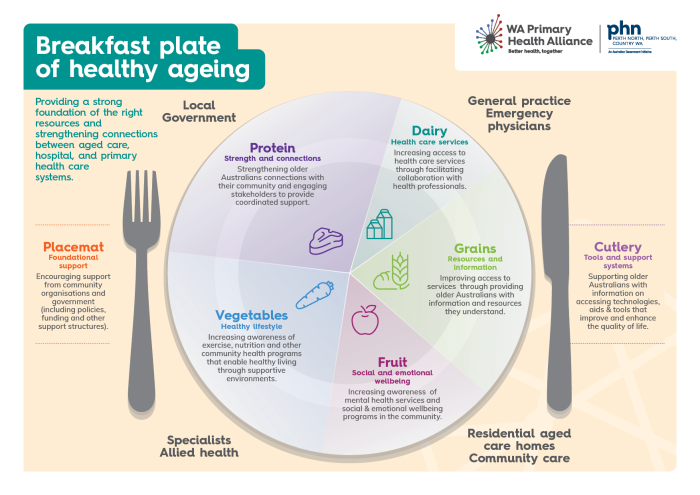
Providing a strong foundation of the right resources and strengthening connections between aged care,hospital, and primary health care systems.
Download a copy of this resource
As the operator of WA’s three Primary Health Networks (PHNs), WA Primary Health Alliance (WAPHA) recognises that transforming services for older people requires a fundamental shift towards care that is coordinated around the full range of an individual’s needs, rather than just diseased focused.
In our Country WA PHN, we bring together the Great Southern Aged Care Network to facilitate a monthly forum for shared, person-centred problem solving and provider system navigation.
This breakfast plate analogy demonstrates how providing older Australians with a strong foundation or ‘healthy breakfast’ of information and resources, and connected community services (across local government, aged care, primary health care providers and hospitals) can improve their access to health care and support them to age healthily within their commuity.
WAPHA led initiatives supporting healthy ageing in our Country WA PHN and across WA include:
• Age Friendly Charter
• Great Southern Compassionate Communities
• Care finders
• Aged care COVID-19 vaccination
• Health Professionals Network
• Online learning to support healthy ageing
Who will GCfAHPC support?
The initiative will support access to palliative care services for people approaching the end of their lives. GCfAHPC will increase patient and carer awareness of palliative care options, including Advanced Care Planning, to facilitate greater community interest in home care support.
WAPHA will also work closely with general practitioners to meet primary care needs and education to increase awareness and access to safe palliative and end-of-life care.
Background
In 2017-18, the Australian Government provided funding to 11 PHN trial sites to pilot the GCfAHPC measure, which included a pilot program in the Great Southern Region of Country WA PHN. The pilot focused on the implementation of Compassionate Communities, a community-based model to build palliative care awareness and capacity within the community. The successful outcomes of the GCfAHPC Great Southern pilot resulted in the City of Albany establishing a “Compassionate Communities” Charter.
Resources developed during this pilot are available through Palliative Care WA for other Local Government Agencies (LGA’s) or community groups who are interested in developing a Compassionate Communities model. In the 2021-22 Budget, the Australian Government has expanded the GCfAHPC funding to all PHNs in Western Australia for four years to 2024-2025.
The Greater Choice for At Home Palliative Care (GCfAHPC) measure aims to improve awareness of local palliative care options and improve coordination of care across the health, aged care, primary care and palliative care sectors.
WAPHA has received funding from the Australian Government to undertake activities that achieve the following objectives:
- Improve access to palliative care at home and support end-of-life care systems and services in primary health care and community care.
- Enable the right care at the right time and in the right place to reduce unnecessary hospitalisation.
- Generate and use data to support continuous improvement of services across sectors.
- Use available technologies to support flexible and responsive palliative care at home, including in the after-hours.
Who GCfAHPC supports?
The initiative supports access to palliative care services for people approaching the end of their lives. GCfAHPC increases patient and carer awareness of palliative care options, including advanced care planning, to facilitate greater community interest in home care support.
WAPHA is also working closely with GPs to meet primary care needs and education to increase awareness and access to safe palliative and end-of-life care.
Background
In 2017-18, the Australian Government provided funding to 11 PHN trial sites to pilot the GCfAHPC measure, which included a pilot program in the Great Southern Region of Country WA PHN. The pilot focused on the implementation of Compassionate Communities, a community-based model to build palliative care awareness and capacity within the community. The successful outcomes of the GCfAHPC Great Southern pilot resulted in the City of Albany establishing a “Compassionate Communities” Charter.
Resources developed during this pilot are available through Palliative Care WA for other Local Government Agencies (LGA’s) or community groups who are interested in developing a Compassionate Communities model. In the 2021-22 Budget, the Australian Government has expanded the GCfAHPC funding to all PHNs in Western Australia for four years to 2024-2025.
The Australian Government has provided funding to WAPHA to support RACHs with training and equipment to deliver telehealth consultations for residents.
This initiative:
- Provides timely access to specialist telehealth for older people receiving care in RACHs. Further information about specialist video consultations under Medicare can be found here.
- Equip RACHs with the necessary equipment and training for staff to support telehealth services.
- Encourage a GP-led model of care.
Who does this initiative support?
Timely access to primary health care professionals, whether through face-to-face consultation or telehealth, is recognised as an issue for many RACHs. This initiative supports:
- RACHs to have access to adequate telehealth to support access to virtual consultations with GPs and other health professionals.
- People who are residents in RACHs to have improved access to telehealth consultations as appropriate to their needs.
Access the after-hours toolkit for residential aged care homes
WAPHA is supporting RACHs to guide and implement after-hours plans and to educate staff on appropriate health care planning for residents who require after-hours care.
WAPHA is engaging with RACHs and primary care to achieve the following objectives:
- Provide guidance to assist participating RACHs to have appropriate after-hours plans in place.
- Educate participating RACH staff on the after-hours health care options and processes for residents.
- Encourage participating RACHs to implement procedures for keeping residents’ digital medical records up to date, particularly following an episode where after-hours care was required.
- Support engagement between RACHs and their residents’ GPs (and other relevant health professionals), as part of after-hours action plan development.
Who does this initiative support?
This initiative focuses on RACHs as:
- RACH residents can experience deterioration in their health during the after-hours period, but immediate transfer to hospital may not always be clinically necessary.
- Lack of awareness and utilisation of out of hours services provided by GPs and other health professionals may lead to unnecessary hospital presentations.
Some older Australians are entering aged care earlier than they may otherwise need to due to a lack of support for healthy ageing or ability to manage their chronic conditions in the community. WAPHA will commission of early intervention services and models for chronic conditions management that support healthy ageing and reduce avoidable hospital admissions.
Improving health outcomes for older Australian’s (particularly those at risk of poor outcomes) through early intervention programs will be guided by the following objectives:
- Expand existing healthy ageing programs where relevant.
- Support older Australians to live in the community for longer (including those not currently receiving aged care services) through commissioning early intervention initiatives that promote healthy ageing, slow decline, and support the ongoing management of chronic conditions.
- Increase awareness in the primary health care workforce of the needs of the population and the availability of these initiatives.
Who does this initiative support?
This measure will seek to support older adults (65 years and over for non-Aboriginal people and 50 years plus for Aboriginal people) who are living in the community with one or more diagnosed chronic conditions and would benefit from being better connected to psychosocial, health and welfare supports.
WAPHA has commissioned care finder service organisations to form part of the national network of care finders who will support improved integration between the health, aged care and other systems at the local level. Visit our Service Directory or My Aged Care’s help from a care finder webpage to find a provider in your region.
CoTA Australia were involved in the transition to the PHN led care finder program, by sharing knowledge from the national navigator trials. The care finder program forms part of a significant investment in aged care reform in response to the recommendations of the Royal Commission.
Who does this initiative support?
The new service will support eligible people who would not be able to arrange services without intensive support and who do not have family members or friends who can help them with connecting to aged care services and support. The service is available to people 65 years or older (50 years for Aboriginal or Torres Strait Islander people or people) or 50 years or older (45 years or older for Aboriginal or Torres Strait Islander people) on a low income and homeless or at risk of being homeless who:
- Need intensive support to understand and access aged care services as well as to connect with any other supports they need, such as health, housing services, and social supports.
- Could otherwise fall through the cracks due to isolation, communication or cognitive issues, or a history of past experiences with institutions or government.
Background
In response to the Aged Care Royal Commission, the Australian Government committed $7 million through the 2021-22 Budget to extend the Aged Care System Navigator trial. The trials, delivered by COTA Australia and partner organisations, continued until 31 December 2022 when the PHN led care finder Program and specialist navigation supports for Aboriginal and Torres Strait Islander began. Through funding under the national Primary Health Network (PHN) Aged Care Program 2021-2025, WAPHA conducted a care finder program Needs Assessment for Perth North, Perth South and Country WA PHNs in July 2022 to inform an open tender request and service specifications.
WAPHA works to increase the awareness, engagement, and utilisation of aged care clinical referral pathways by local health care practitioners (including GPs, allied health and practice staff) and engage local clinical practitioners, and experts in their development.
We review currents pathways, identify gaps and renew clinical referral pathway topics, health services and assessments for inclusion in localised clinical pathway guidance fit for the care of older Australians.
Who does this initiative support?
The WAPHA clinical referral pathways (Clinician Assist) are designed to be used at the point of care, primarily by GPs but is also available to hospital specialists, nurses, and other health professionals.
In February 2022, WAPHA received guidance on dementia clinical referral pathways. Dementia specific clinical referral pathways have been updated.
Who does this initiative support?
The WAPHA dementia clinical referral pathways are designed to be used at the point of care, primarily by GPs but is also available to hospital specialists, nurses, and other health professionals.
Collaborating with Dementia Australia, WAPHA has established a dedicated dementia support web page that will connect those living with dementia and their carers to reliable, local dementia care information, events, and specialist care.
Who does this initiative support?
The Dementia Community Services and Support Finder assists in navigating national and local resources relating to Dementia care for those living with dementia and their family and carers.
Background
WAPHA worked to identify and develop suitable digital and print dementia consumer resources for those living with dementia, their families and carers. By consulting with WA dementia advocates for the dementia consumer resources project, WAPHA sets out to achieve the shared aims of Dementia Australia to affirm the voice of people living with dementia, families and carers and improve community understanding of dementia through access to clear information. WAPHA also leveraged local relationships with WA organisations such as Alzheimer’s WA, Connect Groups, Carers WA, local government and age friendly strategy supporters to accumulate feedback on the format consumers would like to receive information at the point of care from their GP.
WAPHA is engaging with participating RACHs to establish and fund a dedicated clinical coordinator role within RACHs to liaise with GPs, co-ordinate case conferencing and engage GPs in RACH quality improvement.
The intended outcomes of the project will be to:
- Improve resident and family/carer access to primary care and quality end-of-life and palliative care.
- Improve coordination of primary care in RACHs.
- Manage residents’ end-of-life and palliative care health needs to include access to timely and appropriate medication.
- Implement systems and processes to support the sustainable delivery of primary care coordination for general practice and RACHs.
This activity has been made possible through the WA Department of Health NPA Grant. A summary of the 2021 GP consultation key themes: current interaction with palliative care, case conferencing, additional GP support and funding recommendations that informed the project is available here.
To better support older Australians living in residential aged care to receive continuous, quality primary care services from a regular general practice and GP, a new MyMedicare General Practice in Aged Care Incentive has commenced.
Eligible providers and practices registered with MyMedicare are able to receive quarterly incentive payments for meeting the General Practice in Aged Care Incentive eligibility and servicing requirements.
Other useful links and information
WA Primary Health Alliance has a key role in supporting WA residential aged care homes (RACHs) and the primary health providers who in-reach to these facilities in their preparedness and response to COVID-19 general management.
The Australian Government is working with the aged care sector to ensure all residents have access to COVID-19 vaccinations.
Residential aged care providers play an important role in ensuring vaccines are available to residents.
We will improve outcomes for older Australians in WA by:
- Commissioning services for older people which address identified needs and gaps in our PHNs’ local primary health and aged care systems.
- Enhancing access to general practitioners and other primary care providers.
- Improving coordination, integration and continuity of care that contributes to improvements in the health and wellbeing of older people and promotes healthy ageing in place.
- Supporting access to aged care services and other relevant supports in the community and building the capacity of health and aged care professionals to deliver high quality care.

Links and resources:
- My Aged Care
- Australian Government Aged care reforms
- Supporting Healthy Ageing: The Role of PHNs
- Australian Government Ageing and Aged Care Engagement Hub
- Final Report: Royal Commission into Aged Care Quality and Safety
- Volunteering in aged care – Australian Government Department of Health, Disability and Ageing
Education:
- Ageism Online Learning Module
- Recognising, Responding and Reporting the Abuse of Older People
- Medication Management E-Learning
- The Australian Immunisation Register
- Watch on demand: Accessing the Australian Immunisation Register and My Health Record in Aged Care
- Watch on demand: Immunisation in Aged Care and the General Practice Aged Care Incentive